DEXA Body Composition Testing
What is DEXA body composition testing?
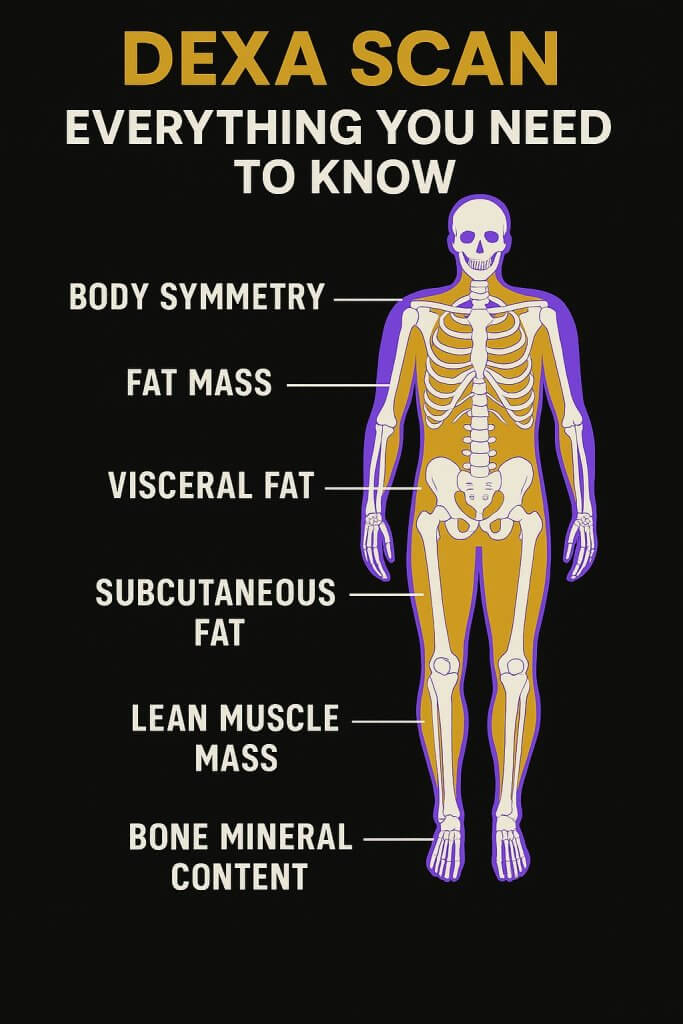
Imagine being able to track all elements of your body composition as you make changes to your diet and exercise plan. DEXA body composition testing is now the new gold standard. Dual-Energy X-Ray Absorptiometry (DEXA). DEXA is the most accurate method for body composition analysis trusted by doctors, medical researchers, and sports labs around the world. Based on a three-compartment model that measures bone mineral content, fat mass (FM) and fat-free mass (FFM), it is fast and non-invasive. DEXA body composition has been regarded as the gold standard measurement tool for its accurate and reliable results. For those who are considering a weight loss journey or a customized fitness program, a DEXA scan provides an important baseline. Most are surprised with the motivation that real metrics provides to track progress and make changes for a healthier lifestyle.
So what does your personalized DEXA test report tell you? Outlined in this report is your android/gynoid ratio, body fat percentage, lean tissue mass percentage, resting metabolic rate, distribution of muscle, fat, bone and much more.
Why consider a DEXA Body Composition?
- Working on managing your weight, and need to monitor your body fat loss and muscle growth under a customized exercise plan.
- Interested in reducing your risks of heart disease, diabetes, high blood pressure, high cholesterol, cancer, and obesity. A DEXA test is a great first step in the right direction to manage your risk profile.
- An athlete and/or bodybuilder who must keep track of muscle building and bone health during training and recovery periods. Jumping on the conventional scale does not tell you everything you need to know about your body to make better and more informed decisions about your health. Contact our team of experts at Push Pounds Sports Medicine to learn more about how you can incorporate DEXA body composition testing to track the impact of your healthy lifestyle.
Cost of DEXA body composition testing?
- 1 Scan – $85
- 2 Scans – $150 (does not expire)
- Any additional – $75 (3 or more)
How is RMR calculated?
There are three possible ways that the DXA RMR result can be calculated. This is the explanation that comes from the operator’s manual and note that there are three ways to calculate RMR: Harris-Benedict[1], Mifflin-St. Jeor[2] or enter manually.
The Harris-Benedict equation is:
RMR(male) = 66.473 – (6.775 x age[yrs]) + (13.7516 x weight[kg]) + (5.0033 x height[cm])
RMR(female) = 655.0955 – (4.6756 x age[yrs]) + (9.5634 x weight[kg]) + (1.8496 x height[cm])
where weight is the entered patient weight.
The Mifflin-St. Jeor formula is:
413 + 19.7 x FFM (kg)
where FFM (Fat Free Mass) = Lean mass (kg) + Bone mass (kg)
[1] Harris JA, Benedict FG. A biometric study of basal metabolism in man. Washington, DC: Carnegie Institute of Washington, 1919. (Carnegie Institute of Washington Publication 279)
As you can see, only the Mifflin-St Jeor method uses the DXA results.
Patient instructions and FAQ:
A client’s scan begins with a 15-minute consultation with our doctor to review all of your goals, answer any questions you may have, obtain consent and provide you with your referral. You will then perform the DEXA right after, which will take an additional 15-minutes for the test and review of results with our doctor.
If you have never had a scan, we recommend our clients to get the 2 scans so that you can have a before and after comparison to evaluate any programming you may be doing.
The DEXA scan generally takes a total of 30 minutes to complete. It is totally painless and the process is very straightforward. DEXA utilizes a very low dose x-ray equivalent to the amount of radiation you would receive while on a flight to New York City. Different from other types of tests such as MRIs or CT scans, there is no oppressive, closed tunnel or ring. Simply lie on your back, breathe comfortably and relax. The scanner does the rest. When finished our team will review your results. We will also provide you with your detailed report to take home.
Please wear or bring with you loose athletic clothing (no metal). For best accuracy of your measured weight, try not to eat a large meal immediately prior to the test. For example, for a morning test, you may want to test before having a large breakfast. In the afternoon, test before having lunch and in the evening, test before having a large dinner.
We also try to offer same day appointments for all clients and we are open 9 am – 8 pm Monday to Friday. Our phone number is 416-722-3393. We look forward to hearing from you, please request your consultation today!
Disclaimer: Do not treat this as medical advice as it is used for educational purposes only. Please seek out help from one of our health care professionals.
1. What is a DEXA scan and how does it work?
A DEXA (Dual-Energy X-ray Absorptiometry) scan is an enhanced X-ray technology using a C-arm apparatus. It sends two low-dose X-ray beams with distinct energy peaks through the body. One peak is absorbed mainly by soft tissue, the other by bone. A detector measures how much of each beam passes through. Computer software subtracts the soft tissue absorption, calculating the remaining bone mineral content and density (BMD), often expressed as g/cm². This relies on the different ways tissues weaken the X-ray beams.
2. What are the main uses of DEXA scans?
DEXA scans have two primary applications: assessing bone mineral density (BMD) and analyzing body composition. It’s the main tool for diagnosing osteoporosis and osteopenia by measuring bone loss. For body composition, it quantifies fat mass, lean soft tissue (muscle, organs), and bone mineral content for the whole body and specific regions. This dual capability provides a holistic health view, useful in various medical fields.
3. Why is DEXA considered a “gold standard”?
DEXA is widely called the “gold standard” primarily for measuring Bone Mineral Density (BMD) and diagnosing osteoporosis. This status comes from its proven accuracy, high precision (reproducibility), ability to measure key fracture sites (hip, spine), and extensive validation. For body composition, it’s considered a clinical gold standard, more accurate than methods like BIA or skinfolds. While research uses more complex models or MRI/CT for specific tissues, DEXA offers the best balance of accuracy, detail, cost, speed, and low radiation for routine clinical use.
4. How does DEXA help diagnose and monitor osteoporosis and osteopenia?
DEXA is the primary tool for diagnosing osteoporosis (severe bone loss) and osteopenia (low bone mass). It detects small reductions in bone density early, often years before a fracture occurs, allowing for timely interventions like lifestyle changes or medication to prevent further bone loss and fractures. DEXA is also highly effective for monitoring bone density changes over time, tracking disease progression, or assessing the effectiveness of osteoporosis treatments.
5. How does DEXA assess fracture risk?
DEXA assesses fracture risk primarily through Bone Mineral Density (BMD) measurements at the hip and spine, as lower BMD strongly correlates with higher fracture risk. However, BMD isn’t the only factor. Tools like FRAX integrate DEXA’s femoral neck BMD with clinical risk factors (age, prior fracture, smoking, etc.) to calculate a 10-year fracture probability. Additionally, Vertebral Fracture Assessment (VFA) using DEXA can detect existing spine fractures, and Trabecular Bone Score (TBS) provides insight into bone microarchitecture quality, further refining risk assessment.
6. What other bone-related conditions can DEXA help assess?
Besides osteoporosis, DEXA monitors bone loss from secondary causes like endocrine disorders (hyperparathyroidism), inflammatory conditions (rheumatoid arthritis), malabsorption syndromes, chronic kidney/liver disease, and certain medications (glucocorticoids, some cancer treatments). It’s used in pediatrics for conditions affecting bone growth (rickets, osteogenesis imperfecta). Opportunistically, it can detect Abdominal Aortic Calcification, indicating cardiovascular risk. It’s also used pre-operatively in orthopedic surgery (hip/spine) to assess bone quality, potentially influencing surgical plans.
7. How are DEXA bone density results reported (T-scores and Z-scores)?
DEXA reports Bone Mineral Density (BMD) in g/cm². Clinically, results use T-scores and Z-scores. The T-score compares BMD to a healthy young adult (same sex) and is used for diagnosis in postmenopausal women and men 50+. Normal is ≥ -1.0, osteopenia is -1.0 to -2.5, osteoporosis is ≤ -2.5. The Z-score compares BMD to age-matched peers and is used for premenopausal women, men <50, and children. ≤ -2.0 is “below expected range for age”.
8. What information does a DEXA body composition report provide?
A DEXA body composition report details fat mass, lean soft tissue mass, and bone mineral content in kilograms or percentages, for the total body and regions like arms, legs, trunk, android (waist), and gynoid (hips). It often includes derived metrics like Visceral Adipose Tissue (VAT) estimate, Android/Gynoid (A/G) ratio for fat distribution, Fat Mass Index (FMI), Fat-Free Mass Index (FFMI), Appendicular Lean Mass Index (ALMI) for sarcopenia risk, estimated Skeletal Muscle Mass (SMM), and estimated Resting Metabolic Rate (RMR). Visual maps often show tissue distribution.
9. How are DEXA body composition results compared to reference ranges?
DEXA body composition results are contextualized using reference data, often presented as percentiles compared to age- and sex-matched peers (AM percentile) or sometimes a young normal group (YN percentile). However, universal reference ranges are challenging due to variations between DEXA manufacturers (GE, Hologic), software versions, and reference databases. Indicative ranges exist: e.g., elevated VAT risk around 100-160 cm²; lower A/G ratio risk <0.8 (F) / <1.0 (M); sarcopenia risk ALMI <5.5 (F) / <7.0 (M) kg/m²; suggested healthy FMI 5-9 (F) / 3-6 (M) kg/m². Interpretation requires knowing the specific reference data used.
10. How long does a DEXA scan take and what is the procedure like?
A DEXA scan appointment is typically short, with the scan itself taking 10 to 30 minutes, depending on the machine and areas scanned. Some body composition scans might be faster, around 7 minutes. During the procedure, the patient lies comfortably on their back on a padded table. An X-ray generator is below, and a detector arm moves slowly above. Precise positioning is crucial. The patient must remain still and may hold their breath briefly. The process is non-invasive and painless.
11. How should a patient prepare for a DEXA scan?
Preparation is minimal. Wear loose, comfortable clothing without metal (zippers, belts, underwire bras). Remove metal objects like keys and jewelry. You might need to wear a gown. Stop calcium supplements 24-48 hours before the scan. Inform staff about recent contrast studies (barium, CT contrast, nuclear medicine scans), as a waiting period (days to 2 weeks) may be needed. Usually, no fasting is required for bone density, but some body composition scans may require fasting. Inform staff if possibly pregnant.
12. Is the radiation from a DEXA scan harmful?
The radiation dose from a DEXA scan is extremely low and considered very safe. It’s often compared to less than one-tenth the dose of a standard chest X-ray or similar to the natural background radiation received in a single day. The effective dose is estimated at less than 10 microSieverts (µSv) or around 0.001 milliSieverts (mSv). The associated health risk is minimal, and the diagnostic benefits typically far outweigh this small risk for indicated patients. Radiation does not remain in the body afterward.
13. When should a DEXA scan not be performed (contraindications)?
The main absolute contraindication for a DEXA scan is known or suspected pregnancy, due to potential risks to the fetus from radiation. Scans should also be postponed if the patient has recently received radiographic contrast agents (like barium or CT contrast) or nuclear medicine tracers, as these interfere with accuracy. Patients exceeding the specific DEXA table’s weight limit (which varies, e.g., 300 lbs up to 225 kg) cannot be scanned. Additionally, individuals unable to lie flat, achieve correct positioning, or remain still may not be suitable candidates.
14. How often should DEXA scans be performed?
Frequency depends on the purpose. For bone health monitoring, Medicare often covers scans every 24 months, but annual scans might be needed for new treatments or rapid bone loss. Guidelines suggest 1-2 year intervals for monitoring treatment. For low-risk individuals, intervals could be much longer (4-15 years). For young, low-risk premenopausal women, 5-10 years might suffice if risk factors don’t change. For body composition tracking (fitness/wellness), there are no set guidelines. Quarterly or semi-annual scans might be desired, but cost, radiation, and potential inaccuracies with short intervals are considerations.
15. Who should be screened for osteoporosis using DEXA?
Screening guidelines primarily target osteoporosis risk. Key recommendations include: women aged 65+; postmenopausal women <65 with increased risk factors (identified via tools like FRAX); men aged 70+; men 50-69 with risk factors; adults with a fragility fracture; adults with conditions/medications causing bone loss (e.g., steroids, rheumatoid arthritis); and those starting/monitoring osteoporosis treatment. Other factors include significant height loss, family history, smoking, low body weight, and certain diseases. USPSTF finds insufficient evidence for routine screening in men.
16. How does DEXA compare to other methods for bone density assessment?
DEXA is the standard for diagnosing osteoporosis. Quantitative CT (QCT) measures true volumetric density and trabecular bone but has higher radiation and cost. Quantitative Ultrasound (QUS), often at the heel, is portable, radiation-free, and cheaper but less accurate for predicting hip/spine fractures and cannot use WHO T-score criteria. Standard X-rays are insensitive to early bone loss. Nuclear Bone Scans detect metabolic activity (fractures, cancer, infection) but not density. DEXA offers the best balance of accuracy, precision, low radiation, and availability for BMD assessment.
17. How does DEXA compare to other methods for body composition assessment?
DEXA provides a 3-component analysis (fat, lean, bone) and regional data. It’s more accurate than Bioelectrical Impedance Analysis (BIA) and skinfolds, which are cheaper but less reliable and sensitive to factors like hydration. Hydrostatic Weighing and Air Displacement Plethysmography (BodPod) are lab methods but are less practical and rely on assumptions. MRI and CT are research gold standards for specific tissue quantification (like visceral fat) but are expensive, less accessible, and CT involves significant radiation. DEXA offers a good balance of accuracy, detail, practicality, and low radiation for many clinical/performance uses.
18. What factors can affect the accuracy and reliability of DEXA scans?
Accuracy depends on machine calibration/quality control; results vary between manufacturers. Operator technique is crucial; incorrect patient positioning or analysis (ROI placement, excluding artifacts) causes errors. Patient factors like movement, extreme body size (very thin/obese), underlying bone issues (arthritis, fractures, surgery) falsely altering BMD, and external/internal artifacts (metal clothing, implants, contrast media) interfere. Significant weight changes can also bias longitudinal body composition tracking. Rigorous protocols are essential.
19. How does hydration status affect DEXA body composition results?
DEXA assumes lean tissue has constant hydration (~73%). Significant changes in hydration (dehydration or overhydration/edema) can alter lean tissue’s X-ray attenuation. This can lead to misclassification, primarily affecting the lean mass estimate and, consequently, the fat mass calculation. While DEXA is less sensitive to hydration than BIA, maintaining consistent hydration before serial body composition scans is recommended to minimize variability and improve the reliability of tracking changes over time, especially for athletes or those with fluid balance issues.
20. How do metal implants or joint replacements affect DEXA scans?
Metal implants (hip/knee replacements, spinal hardware) significantly interfere with DEXA accuracy. Metal causes artifacts and drastically overestimates Bone Mineral Content (BMC) and Density (BMD) in the affected region. Therefore, BMD assessment at sites with metal is unreliable; the site should be excluded or the opposite limb scanned. The impact on soft tissue (fat/lean mass) seems less severe but is inconsistent; some studies show minimal effect after adjustments, while others report overestimated lean mass. DEXA might still track changes over time if the implant is stable.
21. How do breast implants affect DEXA scans?
Silicone breast implants act as artifacts, significantly attenuating X-rays. Studies show implants cause substantial overestimation of bone area, BMC, and BMD, especially in the trunk and total body measurements. This can artificially inflate spine BMD readings, potentially masking osteopenia or osteoporosis and leading to missed diagnoses. Effects on soft tissue (fat/lean mass) are less consistent, with some studies finding significant increases and others only small, potentially insignificant changes in the trunk. Clinicians should be aware and may rely more on unaffected sites (hip, forearm).
22. How precise and reproducible are DEXA measurements?
DEXA is considered highly precise (reproducible) when performed correctly. Precision is measured via repeat scans to calculate the Least Significant Change (LSC) – the minimum change needed to be statistically significant. ISCD sets minimum precision standards for technologists (e.g., LSC ≤5.3% for spine BMD). Body composition precision is also good, with low coefficients of variation (CV%) reported for total fat (0.9-1.9%), lean mass (0.5-1.0%), and BMC (0.5-0.8%), though values vary by machine. High precision allows reliable tracking of changes over time.
25. Is a physician referral needed for a DEXA scan?
For medically indicated bone density scans, especially for insurance coverage, a referral/order from a healthcare provider is usually required to establish medical necessity. For elective body composition scans (self-pay for wellness/fitness), requirements vary. Some specialized clinics offer direct access without a referral. However, other facilities might still require a provider’s order even for self-pay scans. Patients obtaining scans directly should consider sharing results with their primary provider for clinical context.
26. How is DEXA body composition linked to health outcomes?
DEXA provides metrics linked to health risks. High Visceral Adipose Tissue (VAT) is strongly associated with cardiovascular disease, Type 2 diabetes, and metabolic syndrome. Central fat distribution (high Android/Gynoid ratio) also indicates higher metabolic risk. Low muscle mass (sarcopenia), assessed via ALMI or FFMI, is linked to poor function, falls, frailty, and higher mortality. DEXA accurately tracks fat vs. lean mass changes during weight management, crucial for preserving muscle. It’s also used in conditions like HIV-lipodystrophy and cancer cachexia.
27. How is DEXA body composition relevant to athletic performance?
DEXA is valuable for athletes. It accurately tracks changes in muscle (lean mass) and fat mass from training and nutrition. Regional analysis identifies muscle imbalances or asymmetries between limbs, which can inform corrective training and potentially reduce injury risk. It helps athletes optimize body composition (fat percentage, lean mass) for their specific sport. DEXA also monitors bone density, important for athletes at risk of low BMD (e.g., female athlete triad, RED-S) to prevent stress fractures. Its precision allows tracking small but significant changes.
28. What are the main advantages of DEXA scans?
DEXA offers high accuracy and precision for both bone density (gold standard) and body composition (clinical standard). It provides a comprehensive 3-component analysis (bone, fat, lean) with regional data, including visceral fat estimates. The procedure uses a very low radiation dose, is non-invasive, quick, and painless. Standardized criteria (T-scores) exist for osteoporosis diagnosis. It enables early detection of bone loss and effective monitoring of treatments.
29. What are the main disadvantages and limitations of DEXA scans?
Limitations include cost and potentially limited accessibility, especially for uninsured/elective scans. While low, it uses ionizing radiation, a concern for frequent scans. Accuracy is affected by artifacts (implants, arthritis), operator technique, body size extremes, and hydration changes. It measures areal, not true volumetric, BMD. Lack of standardization between manufacturers hinders direct comparison of results. It identifies low density/composition issues but not their underlying cause and provides risk estimates, not definitive fracture prediction.
30. Is a DEXA scan covered by OHIP?
DEXA scans performed for medical purposes (such as diagnosing or monitoring osteoporosis) are covered by OHIP when ordered by a physician and deemed medically necessary.
However, body composition DEXA scans (those used for tracking fat, muscle, or visceral fat changes for wellness or athletic goals )are not covered by OHIP.
31. Is a DEXA scan free?
DEXA scans for body composition or wellness assessments are not free. OHIP coverage applies only to medically indicated bone density scans ordered by a healthcare provider.
For personal health, sports, or wellness purposes, scans are self-pay and competitively priced — for example:
- 1 Scan – $85
- 2 Scans – $150 (does not expire)
- Additional scans – $75 each (3 or more)
32. What should you never do before getting a DEXA bone scan?
Avoid taking calcium supplements for 24–48 hours before your scan, as calcium can interfere with results.
Do not undergo the test if you’ve recently had any barium studies, CT contrast, or nuclear medicine scans, as these can distort accuracy.
You should also avoid wearing metal (zippers, belts, underwire bras, or jewelry) and refrain from heavy meals immediately before testing for the most accurate readings.
33. Who qualifies for a DEXA scan?
DEXA scans are recommended for:
- Women aged 65+ and men aged 70+
- Postmenopausal women or men over 50 with risk factors for osteoporosis (like family history, low body weight, or prior fractures)
- Adults with chronic conditions or medications that affect bone health (e.g., steroid use, rheumatoid arthritis)
- Athletes and individuals seeking detailed body composition tracking
For general fitness or wellness purposes, any adult can self-book a DEXA body composition scan.
Which patients should not have a DEXA scan?
DEXA scans should be avoided during pregnancy due to radiation exposure. They are also not recommended immediately after contrast imaging (barium or CT), or for patients unable to lie flat or remain still. Individuals over the machine’s weight limit cannot be scanned safely.
34. Can I self-refer for a DEXA scan?
Yes, for body composition scans you can book directly without a physician referral. These are elective wellness tests, and you can contact the clinic to schedule your appointment. For bone density scans performed for medical diagnosis, a doctor’s referral is required to qualify for OHIP coverage.
35. What’s the difference between a bone density scan and a DEXA scan?
Technically, they’re the same technology. A bone density scan is a type of DEXA scan specifically focused on measuring bone mineral density (BMD) to assess conditions like osteoporosis. A DEXA body composition scan, on the other hand, analyzes fat mass, lean mass, and visceral fat, providing a complete picture of overall health beyond bone density alone.
36. Can I drink coffee before a DEXA scan?
Yes, you may have coffee before your scan, but it’s best to avoid large meals or excessive fluid intake immediately beforehand. Caffeine itself does not interfere with DEXA accuracy, though testing on a consistent schedule (same time of day, similar routine) can help ensure reliable comparisons across visits.
37. What to do the night before a DEXA scan?
The night before, simply follow your normal routine. Avoid taking calcium supplements, and ensure you are well hydrated.
Try to keep your diet and fluid intake consistent if you plan to compare results over time. There is no fasting required, but avoid alcohol or excessive salt intake, as both can temporarily alter body fluid balance.
38. Is a DEXA scan done on an empty stomach?
Not necessarily. You can eat normally, though it’s recommended to avoid large meals within two hours of your scan. Testing under consistent conditions (like before breakfast or before lunch) helps maintain reliable data over time.
Can I eat yogurt before a DEXA scan?
Yes, you can eat yogurt before your scan, but avoid large meals immediately prior. Foods rich in calcium, like yogurt, should be avoided within 24 hours only if you are having a bone density test, as calcium can slightly affect bone reading results. For body composition scans, it’s fine to eat lightly before your appointment.
Should I be fasted for a DEXA scan?
Fasting is not required for a DEXA scan. However, for the most consistent results ( especially if you are tracking body composition over time ) it’s best to test under similar conditions each time (for example, before breakfast or a few hours after your last meal).
Does drinking water affect DEXA?
Mild hydration differences have minimal effect, but drinking excessive water right before the scan can slightly alter lean mass readings since DEXA assumes constant tissue hydration. For best results, maintain consistent hydration between repeat scans.
39. What is the best time of day for a DEXA scan?
Any time of day is acceptable. However, if you’re doing multiple scans for progress tracking, it’s ideal to schedule them around the same time of day, since hydration and food intake can slightly affect results.
40. Do you get DEXA scan results immediately?
Yes. Your scan results are typically available right after your appointment. The technologist or physician will review your report with you, explain key findings like body fat percentage, lean mass, and visceral fat, and provide you with a detailed printout or digital copy to take home.
41. What to wear before DEXA scan
You can remain fully dressed during your DEXA scan, as long as your clothing is light, comfortable, and free of any metal components. Avoid items such as zippers, buttons, snaps, or metallic threads, since these can interfere with image quality. Loose-fitting athletic wear like a T-shirt and lightweight shorts or leggings is ideal and ensures accurate results without the need to change.
Leggings are perfectly acceptable for a DEXA scan, provided they don’t contain metal fibers or decorative zippers. Many people find them comfortable and easy to move in, which helps maintain proper positioning during the scan. Similarly, socks can be kept on throughout the procedure as they don’t affect the scan in any way.
When it comes to undergarments, non-metallic sports bras or soft fabric bras without underwire are recommended. Metal underwire bras, clasps, or decorative elements can distort readings and may need to be removed. If your clothing does contain metal and cannot be easily changed, the technologist may ask you to wear a clinic-provided gown to ensure scan accuracy.
Overall, the goal is to wear lightweight, metal-free, and comfortable clothing so you can relax during the short, painless scan and obtain the most accurate body composition or bone density results possible.
42. Is a DEXA scan considered nuclear medicine? Is it a lot of radiation?
Not at all. The radiation dose is less than one-tenth of a chest X-ray and roughly equal to what you’d experience on a short airplane flight. It’s one of the lowest radiation exposures among all imaging tests.
43. Can I take vitamin D before a DEXA scan?
Vitamin D does not affect DEXA scan results, so you can take it as usual before your appointment.
44. Can I take Tylenol before a DEXA scan?
Tylenol and other pain relievers do not interfere with the scan and may be taken normally.
- 55 University Avenue, Mezzanine Floor, M002, Toronto, ON, M5J 2H7, (416)7223393, Toronto DEXA body composition

